A.I. in the Future of Healthcare...from a Concerned Patient
Artificial Intelligence (A.I.) has been the biggest technology buzzword since the IoT/Big Data era and is an especially hot topic within healthcare right now, but most people still have no idea what it actually encapsulates.
What is AI…at a very high level
So, how is AI defined? Apart from a computer powered Arnold Schwarzenegger, A.I. is commonly quantified in a few buckets that were made famous by the Turing Test proposed in 1950 by famous scientist, mathematician, and Nazi code breaker Alan Turing. [1]
Turing suggested at the time that to be intelligent in the same way we view human intelligence a computer would need to possess the following abilities: [1]
Natural Language Processing - the ability to communicate successfully in a language of choice
Knowledge Representation - the ability to store and retain the information received
Automated Reasoning - the ability to use stored information both to answer questions and to further reason to draw new conclusions
Machine Learning - the ability to detect and extrapolate patterns, adapting to new circumstances as they arise
The following physical characteristics have since been added that while unnecessary in defining intelligence are often grouped into the study and development of artificial intelligence: [1]
Computer vision - the ability to perceive objects
Robotics - the ability to manipulate objects and move according to its surroundings
As you can see, while often used as a separate buzzword interchangeably with AI, Machine Learning actually describes a sub-section of AI and even within that there are multiple learning approaches such as unsupervised and reinforcement learning. More complex concepts including, but not limited to neural networks (software modeled after adaptable brain neurons) and deep learning (multilayered neural networks that allow the software to train itself) are often directly responsible for making the headline worthy innovations we often see in the news. [2] With this basic context, we can zoom out to the bigger questions: How does this technology plug into the larger healthcare ecosystem?
Applications across Healthcare
“People are at the heart of healthcare – physicians, nurses, clinicians and of course, their patients. We are committed to empowering care teams with the tools they need to deliver their best care as well as empowering people as they interact with various aspects of the healthcare system.”
Peter Lee, Vice President of Microsoft Healthcare
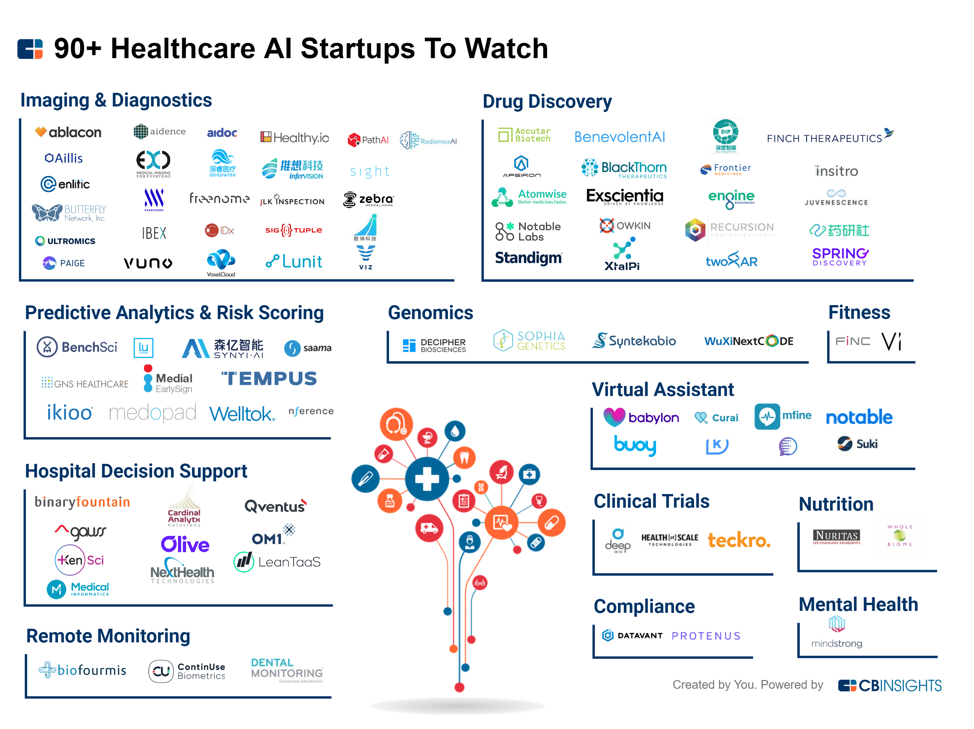
Applications for AI within healthcare are continuously growing as AI solutions become more advanced. Some fields are already becoming differentiated as areas “ready” for an AI revolution, such as the highly pattern focused field of radiology.
Below is a snapshot of Radiology machine learning applications, as mentioned in Eric Topol’s Deep Medicine: [2]
Detecting the texture of brain MRI images to detect a genomic anomaly relevant to surviving types of brain cancer
Performing mammograms with similar accuracy to 23 radiologists in the Netherlands
Helping to avoid more than 30% of existing breast surgeries using mammography images coupled with biopsy results that indicate high risk of cancer
Diagnosing hip fractures with 99%+ accuracy from X-ray images instead of more expensive techniques (MRI, nuclear bone scans, or CT)
Detecting cancerous lung nodules with an accuracy similar to board-certified radiologists and increased total accuracy when combined with their expertise
Detecting vertebral compression fractures with 93% accuracy (radiologists routinely miss such fractures 10%+ of the time)
Detection of bone micro-fractures in musculoskeletal scans when the fracture was as small as 0.01% of the X-ray image
These existing applications are far from a turn-key radiology solution and even in their current form are often confined within academic forums rather than real-world settings. However, these examples are the tip of the iceberg when it comes to pattern recognition opportunities within healthcare. Other pattern driven “doctoral” functions include pathology and dermatology, but pattern-focused applications become even more evident as we expand our scope. [2] Other areas with immense data sets in biomedicine — such as genomics and drug discovery and development — are also ripe for this kind of disruption. A.I. solutions are already being used to draw new insights by processing immense amounts of data faster than human led R&D efforts are capable of.
Robotic surgery is another important area for disruption. In 2017, a headline broke about a motion-controlled robot performing microsurgery, but underneath the surface A.I. was at work. The procedure was aimed at correcting lymphedema using a microsurgery procedure that requires suturing vessels as small as 0.3 millimeters across. This is a difficult procedure for even the best of surgeons, but using artificial intelligence features, the robotic device was able to mimic surgeon hand motions and reduce the surgeon’s unsteady movements to perform the procedure with increased precision. [4] This is just the beginning of A.I.-assisted surgical robotics. Other applications are underway for both standard and complex procedures to help reduce surgical complications and errors.
Implications for Doctors
At first glance, medical practitioners appear to face a bleak future. As data sets become more robust and A.I. solutions become more sophisticated, what role will human doctors have left to play? However, the future doesn’t need to be bleak. For example, consider the radiological field. There are approximately 40,000 radiologists reviewing 800 million annual scans. [2] This overwhelming ratio is a large reason why 31% of American radiologists have faced a malpractice claim. [5] What if machine learning solutions could help review images with radiologist supervision? Radiologists may be able to cover more images, may be able to spend more time on more ambiguous images, and perhaps most importantly radiologists would have more time to discuss the results with the patients. This is a great example of how practitioners will need to communicate their value moving forward — as “partners with A.I.” [2]
Practitioners will need to show their value as medically trained supervisors of machines, and amplify the human aspect of care patients receive.
Other applications of A.I. will be targeted specifically towards the goal of freeing practitioner time to focus on patients. For example, creating virtual nursing assistants that can free up time spent by doctors and nurses on maintenance tasks by using natural language processing (NLP) to record initial patient verbal responses and turn answers into useful text data. [6] These tools will allow medical practitioners to spend more of their time on complex tasks and providing more individualized patient care.
Concerns
AI applications are often created with a data set in mind. In and of itself this isn’t a problem, because as data increases the applications will continue to learn and should be able to be changed. However, therein lies the problem, AI solutions are created by errant humans and often are a black box. Kate Crawford, a co-founder of a research group working for Microsoft Research, said last year "You cannot have black box systems in core social services." [7] Many find themselves on both sides of the argument, especially when tools appear to work.
However, many AI applications have already been found to be discriminatory. A good example comes from a 2016 ProPublica study on predictive policing risk assessments. [8] The focus of the study is largely centered around a Northpointe software used widely throughout the country, and isolating for other variables they found a positive correlation between black convicts and higher scores. While this tool was made with good intentions, it inadvertently furthered systematic racism. As new A.I. models are introduced in health insurance, auto insurance, and other fields, conversations around the tools’ implications for equality will deepen.
Another looming question with A.I. centers on data privacy. What data is truly private? As we freely give away data on social media, we many times don’t have explicit ownership over our own personal data. For example, surveillance systems used by the Chinese government use biometric data picked up by surveillance systems in countries across the world every day. [9] As more and more data is collected and advanced AI solutions emerge, access to our personal data and control over how it is shared and used will become increasingly important. Advanced cybersecurity measures will be vital to protect data from bad actors, but we will also need to be proactive to help individuals know how to shepherd their data and to advocate policies that protect this data.
Potential Future
“One of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.”
Dr. Francis W. Peabody, Harvard Medical School
It is hard to fully comprehend what the current landscape will mean for how healthcare is provided in the future. Some experts think that all A.I. innovations will be positive, while some remain more skeptical. This skepticism is evident in a 2017 robotic surgery article, which started by saying, “AI-controlled robots will almost certainly enslave humanity and make us all wish we could go back to the Stone Age.” Right now, the truth is we don’t know what the future will look like or if the result will be a net positive or negative. All we can do is speculate.
To see one potential clinical future for some of these solutions, one need look no further than Guangzhou Hospital. AI solutions used include patient records organization, identification of patients with facial recognition, bot suggested diagnoses, scan interpretation, and operating room workflow. [5] Medical facilities will continue to adapt and update much like the facility in Guangzhou, adding more solutions to facilities as they progress. We may even be moving toward a future where services are conducted from the comfort of one’s home. With the proliferation of consumer friendly NLP tools such as Alexa and Siri, it is no longer unimaginable to have a personal in-home assistant that can serve many of of the same functions received by A.I-enabled bots in a hospital setting. Such an assistant may be able to conduct quick tests, provide suggestions, offer to schedule appointments, and more. These innovations have exciting implications for accessibility to treatment, uncertain implication for patient outcomes, and concerning implications for on personal data security. It is incumbent on us — patients and practitioners alike — to play an active role in keeping solutions focused on caring for people, and in keeping the future of A.I. in healthcare bright.
About the Author:
JB Stockslager
JB Stockslager is a 1st year MBA student at Kellogg. Before Kellogg, JB briefly spent some time with a private hospital provider in the U.K. before working at A.T. Kearney with executives across a variety of industries including time spent building a heuristic planning algorithm to help bring a client into the digital age and evaluating synergies for a large pharma merger. JB is part of this year’s Business of Healthcare Conference and is passionate about innovative solutions that can help all people gain access to better care.
Sources:
Artificial Intelligence: A Modern Approach
Eric Topol, Deep Medicine (2017)
https://nypost.com/2017/10/04/the-worlds-first-robot-super-microsurgery-was-successful/
S Whang, Jeremy & Baker, Stephen & Patel, Ronak & Luk, Lyndon & Castro, Alejandro. (2012). The Causes of Medical Malpractice Suits against Radiologists in the United States. Radiology. 266. 10.1148/radiol.12111119.
https://hbr.org/2018/05/10-promising-ai-applications-in-health-care
https://www.propublica.org/article/machine-bias-risk-assessments-in-criminal-sentencing
https://foreignpolicy.com/2018/07/24/beijings-big-brother-tech-needs-african-faces/
Francis Peabody, The Care of the Patient https://jamanetwork.com/journals/jama/article-abstract/245777
Source for Images: https://hackernoon.com/ai-in-medicine-a-beginners-guide-a3b34b1dd5d7